By William Appelgate, PhD
For those physician practices that have made the decision to become a Patient-Centered Medical Home, let us first congratulate you on making the commitment to help move our healthcare system towards a focus of patient-centered, population health improvement. No meaningful, long-term transformation of care delivery and patient engagement is possible without the leadership and commitment of the primary care team, and it is the PCMH (and Accountable Care Organization) initiative that are among the most prominent catalysts for that new future.
But making the successful (and profitable) transition to a PCMH is not some simple two-step process. The additional burdens placed on the practice can be complicated and onerous, including changes to practice workflow, new contracting and reimbursement rules, additional reporting requirements, and simply the overall change in mindset can be overwhelming. Among this list of new requirements to address, arguably one of the most critical objectives is to meet (and exceed) the quality standards established by the National Committee for Quality Assurance (NCQA.) For many, the success of the practice hinges on this or similar recognition (such as through URAC, Joint Commission or state-specific medical home designations) as the benchmark for establishing a successful PCMH. It is that recognition that likely pays off for the practice in critically important quality designations, performance bonuses and other financial incentives.
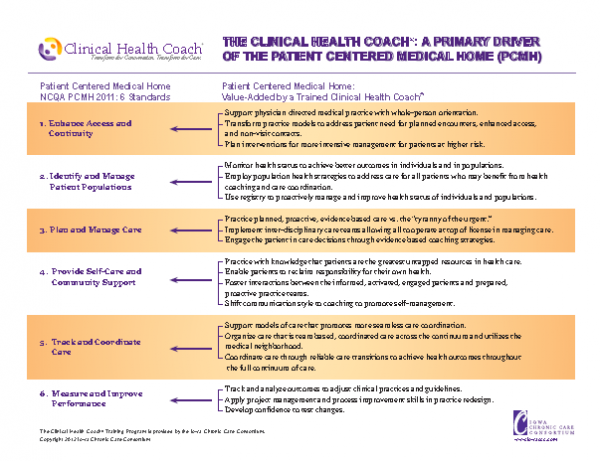
Specifically, NCQA establishes six quality standards that need to be achieved by the practice in order to satisfy recognition requirements. Points are assigned for each category and subcategory, with certain subcategories deemed as ‘Must Pass’ and the number of points earned determining whether the practice achieves a Level 1, 2 or 3 designation.
Of course, if you’re pursuing PCMH recognition, you probably already know all this. But what you may not know is that incorporating a health coach program into the practice workflow can complement and help address each category of the NCQA Recognition Standard. The introduction of a health coach program into your practice can complement and help address each category of the NCQA Recognition Standard. Not only does health coaching contribute positively to the practice revenue equation (a topic we take up in more detail in a future blog post), but an effective health coach program can be among the simplest, most cost-effective investments that a practice can make to meet the NCQA standard.
Admittedly, becoming an effective, profitable PCMH isn’t easy. There are plenty of complicated, expensive and unproven elements that need to be factored in. But health coaching isn’t one of them. Instead, you can start quickly and easily, one staff member at a time. Transform your practice, improve your productivity and your financial effectiveness while you make your way to Level 3. We have included a one-page overview below that details how adding a health coach to your practice can help you achieve NCQA PCMH recognition.
And again, thanks for helping move healthcare toward a future of population health.
[…] from planned, proactive, and population-based strategies, and that those organizations need an effective framework in which to integrate these enhanced communication and engagement skills if they want to impact […]